- Attitudes and behaviours
- Community-led approaches
- Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
14.8k views
Re: Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
This integrated rural water and sanitation project builds on the experiences of the Trust, CInI and its Implementing Support Agencies (ISA) derived from the implementation of community based drinking water supply systems across rural India. The collaboration with the Gates Foundation will focus on integrating sanitation into the village level action plans; leveraging community groups and structures (for example, women’s self help groups (SHGs), community based organizations and committees like the Village Water and Sanitation Committees) to generate demand, shape social norms and streamline delivery; and leveraging available funds for different components like water supply, environmentally sustainable sanitation, etc. from various ongoing Government programs. The main elements of the project are summarized in the table in the document attached below.
As stated previously, Gates Foundation funding will be utilized only to promote sanitation outcomes hence this project will focus mainly on the sanitation component of the project (and related cross-cutting themes).
My response:
This short description talks about 'leveraging' existing efforts, so this is not the same thing at all.
I am often asked if people in villages have not got too many groups to attend and why would we want to start another, with the implication that we are burdening the poor recipients.
Well, in fact if you want to develop core values I think you will succeed better if you start off fresh with a certain vision. If you take a micro enterprise and graft a CHC on top of it I guess it could 'work', but the leader may not be the type to be a CHC facilitator. I think you start from scratch and promote the 'vision' and attract a following... who come for the 'right' reasons' i.e. the 'objective' of the club, which is to prevent common disease, rather than make money for example.
Practically, I can say that we have seldom had the idea refused at village level, and few people have said, 'We don't want this' because we are too busy. If we put ourselves in their position - Would you be happy if you joined a farming cooperative and then were told you were now going to have sessions on hygiene?
Also you notice: the main agenda has already been set by the Donors... improved sanitation. In the CHC we don't set the agenda...we provide a 'forum for debate' on many issues - what comes out is any bodies guess... but very often sanitation is improved. HOwever, it should be noted that sanitation or latrine building is an 'indicator' of behaviour change rather than an 'output' of the programme.
If there are any other examples you want to discuss, I can also help to compare them or debate with others.
Please Log in to join the conversation.
You need to login to replyRe: Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
Why is the CHC (community health club) concept not better known yet? (Hah - maybe it's time to do up a Wikipedia page about it?? What do you think?)
It would be good to have a Community Health Club wiki page.. not sure how that happens.
There is one on Africa AHEAD which I didn't know about...
en.wikipedia.org/wiki/Africa_AHEAD
Is Africa AHEAD the only organisation spear heading it, has your organisation invented it, or have you drawn on somebody else's work?
I was the 'originator' and 'conceptualised' the approach in 1993, and so I guess I would be the leading proponent of this model, although there are lots of enthusiasts who understand it and advocate as well.
Together with my husband, Anthony, a water engineer with long technical experience in hardware, we first started CHC field trials in 1995 in Zimbabwe, funded by Unicef. Anthony is now one of the leading advocates for CHC and together we have founded two organisations, Zimbabwe AHEAD in 1999 and Africa AHEAD 2005 to scale up and replicate regionally. As consultants we have introduced it into 11 countries with 1.5 million beneficiaries purely through the efforts of our advocacy and training.
I did my PhD on the subject of 'Cost-effective hygiene behaviour change through CHCs' based on community uptake of a project that was funded by DFID and Danida from 1999- 2001. I was the first to publish on CHC Model together with Prof Sandy Cairncross in 2005. I was initially inspired by the social science underpinning the Boy Scout Movement but I did not draw on anyone individual work as such.
Who else has picked it up (apart from the Rwanda Ministry of Health)?
We have trained staff of over 30 NGOs to start CHCs and worked with many local and international organisations as partners to implement programmes including the more well known ones: WaterAid, Oxfam, Care International, Mercy Corps, Tear Fund, Action Contra la Faim, IRC, International Lifeline Fund, World Vision, Practical Action. Some NGOs continue to use the approach but there has been no study to see who is doing what and if it is sustainable. As consultants we are rarely told how far the CHC has been taken. More research is needed on how far it has spread in the past 15 years.
We have been funded by DFiD, Danida, USAID, Unicef, EU, Big Lotterly Fund, Gates Foundation...who knows where all the information goes, as there seems to be little institutional memory in these big agencies and it depends who is employed at the time as to whether they understand what has been done. They pick up on it while they are in office and may promote it and the next person forgets it and uses another approach.
Ministry of Health in 8 countries in Africa have requested assistance from Africa AHEAD to introduce it over the past few years as a national programme as we did in Rwanda. These include Zimbabwe, Namibia, Zambia, Malawi, Sierra Leone, DRC, Tanzania, Guinea Bissau. If our expertise came with resources CHC would have been taken up immediately.
Have you had dealings with the health sector, are they using a similar approach?
We always work in partnership with Ministries of Health but usually the Environmental Health Divsion. Until Ministries take preventative health seriously there will continue to be this dichotomy between the two wings of health.
Can you work hand in hand with them, e.g. things like handwashing, behaviour change on breast feeding, food hygiene etc. should all be things that the health sector is also interested in?
Of course, and we continue to advocate for an integrated approach. Our model may be one of the most successful means of achieved the Sustainable Development Goals. Hopefully now development practitioners are talking about 'holistic development' at last, and maybe the various 'sectors' will get out of the tunnel vision prompted by the MDGs and work together. However, it is all about the budget and which Ministry controls it...so until the various Ministries fuse, there is little chance of integrated development. So its a good vision but a little idealistic given the set up on the ground.
Recently in Rwanda major NGOs and MoH are talking about building on the CBEHPP (WASH) programme which which started CHCs in every village to address Nutrition programmes, which are now all the rage. At last planners are beginning to see through the eyes of the community.... what goes in and what comes out of a body obviously belongs in the same programme!
The CHC Model has always addressed the whole range of preventable diseases in our CHC training: not only WASH but nutrition, child care, immunisation, as well as Malaria, Bilharzia, skin disease and worms as part of the 20 topics which are taken in the weekly CHC sessions.
Are similar things perhaps being carried out by others under other names? Like would you say it's similar to the "self help groups" in India? See e.g. here: forum.susana.org/forum/categories/142-go...cini-jharkhand-india
Lots of organisations have realised the power of groups, and for years 'women's groups' have been used and these could be compared, but the 'club' is a bit more structured than this. A member of a CHC has a vision and the training develops core 'values' that result in a 'culture of health' and behaviour change. We also try to attract men and not just for women, as they are 50% of the population who need to improve their hygiene (and change their behaviour) just as much, if not more than women!
Perhaps a CHC is more like a secular Church group. The religions of the world have long known how to get high levels of group solidarity. We copy some of their techniques (in a secular way), singing and dancing, joy and togetherness, emphasis on conformity to an ideal- cleanliness being next to Godliness!
Co-operatives are also quite similar but they are usually for financial gain whereas CHC are a way of life with no material implications. So I guess, a CHC is not a new concept, except maybe in the WASH sector.
I haven't come across any similar programmes which tick all the same boxes. But would be interested to hear with anyone is doing something similar.
Please Log in to join the conversation.
You need to login to replyRe: Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
Thank you for raising the subject of whether Community Health Clubs would work in urban areas...
The short answer is they do! - but you are right in noting that people at work all day cannot always be available during the week for meetings. To get round this, meetings are held in the evening after work.
CHCs tend to be smaller in urban areas (30-60) rather than 70-100 in rural areas and they are held indoors usually at a school or community centre. In many countries in Africa, people tend to drink away their weekends...however one of the advantages sited by a CHC facilitator in eThekwini (South Africa) is that it cut down on drinking hours!
Seriously though, studies (Kawachi) show that in America the more social networks there are in an area, the less stress related diseases such as heart disease, stroke, high blood pressure cancer, eating disorders etc. CHC are one such group, (like a church group) that provide social solidarity particularly to newcomers to town. This can alleviate much suffering and disorientation.
I refer you to our website for more details of where Africa AHEAD has been working in urban context:
africaahead.org/project-type/urban-chc-projects/
In summary:
Zimbabwe: six towns where massive clean up of solid waste were done and relations between council and residents much improved and cholera halted by CHCs in 2009 in one town
South Africa: in urban townships in eThekwini and Cape Town where CHCs were used to get community to cooperate and use public ablution blocks properly
In Vietnam, where the peoples republic took CHCs to a higher level of technology, broadcasting sessions to the whole village with public announcement systems
In Namibia: a pilot for the use of community mobilisation for new ablution blocks in a small town
In DR Congo, where they have recently been well received by desperate communities in war torn peri urban areas.
So I am sure with enough Government support, the CHC could be used to deal with many issues in Ghana related to the pressure of people confined together without proper facilities.
The essence of the CHC Model is that it is a means of community mobilisation, so of course it lends itself to public health issues which require buy in from everyone in the community for standards to improve. Informed group response can be used to improve most situations even more so in urban, and particularly related to water and sanitation and sold waste management.
However, it doesn't end there. Many CHCs start their own saving and loan scheme, child care groups, trading and micro enterprise...
So yes... you should try Community Health Clubs in Ghana... what is there to lose?
Test them and see if they work and let us know.
Please Log in to join the conversation.
You need to login to reply- CaitlinMcC
-
Less
- Posts: 7
- Karma: 1
- Likes received: 1
Re: Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
Very many thanks for these comprehensive and honest answers!
I'd be interested to hear a response to some of Elisabeth's follow-up queries too, particularly your thoughts on whether there are similar approaches to CHC and/or the scope to collaborate with other efforts.
Best wishes,
Caitlin
Please Log in to join the conversation.
You need to login to reply- xonam7
-
Less
- Posts: 3
- Likes received: 1
Re: CHC model in Ghana
The biggest challenges with Sanitation are in the urban slums, and major public areas including markets and slums.
The CHC approach and its successful implementation in Rwanda is very impressive. The pilot studies however seem to have been carried in rural areas.
In your opinion, in busy urban areas where everybody minds their own business and have very little to spend even with their families, do you think CHC model can work? or do you have case studies you can share?
Thank you
Thelma
Please Log in to join the conversation.
You need to login to reply- Elisabeth
-
- User is blocked
- Freelance consultant since 2012
Less- Posts: 3372
- Karma: 54
- Likes received: 932
Re: Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
Thanks very much for your frank and honest answers to Caitlin's questions!
Like Caitlin, I had also wondered:
- Why is the CHC (community health club) concept not better known yet? (Hah - maybe it's time to do up a Wikipedia page about it?? What do you think?)
- Is Africa AHEAD the only organisation spear heading it, has your organisation invented it, or have you drawn on somebody else's work?
- Who else has picked it up (apart from the Rwanda Ministry of Health)?
- Have you had dealings with the health sector, are they using a similar approach? Can you work hand in hand with them, e.g. things like handwashing, behaviour change on breast feeding, food hygiene etc. should all be things that the health sector is also interested in?
- Are similar things perhaps being carried out by others under other names? Like would you say it's similar to the "self help groups" in India? See e.g. here: forum.susana.org/forum/categories/142-go...cini-jharkhand-india
Also you said:
As you said "some countries": which are the other countries? Is it South Africa and Zimbabwe?In some countries, such as Rwanda, Unicef and USAID have supported the model through Ministry of Health and it has gone to scale in a national programme with a CHC now established in almost all the villages in the country.
Furthermore, I have listened to the recording again to see which of the questions from the webinar's chat have been answered verbally and how.
These are:
-Henrietta: How were the 20 topics for community health clubs (CHC) decided upon?
Your answer in the webinar was (please expand if you like):
The topics are related to the context where we are working. For example in urban areas in South Africa there is no malaria and bilharzia, so these two topics were not includced there.
In the design of the program you work with the Ministry of Health for example and identify the topics of relevance.
-Bruce Southerland: In Rwanda are you working through or with local government health agent?
Your answer in the webinar was (please expand if you like):
The program in Rwanda is a national program (Ministry of Health). CHCis seen by the government as an approach for nation building. The program is run by the Ministry of Health; we support them to enable better monitoring and quality control; a RCT (randomised controlled trial) is currently being done by ipa (with Gates Foundation funding)
-Kumi: CHC sounds like an excellent approach. Regarding the latrines, what are club members expected to do with the collected waste over the long term (e.g. when the pit fills up).
Your answer in the webinar was (please expand if you like):
It depends on the context: In urban areas there is a variety of technologies available for emptying pits. In rural areas the community members seal the full pit and dig another pit.
-Penninah: It appears this is a great way to integrate various programs, how many organizations are you working with, have they documented successes? are they sharing and where can we find the documents?
Answer from Juliet Waterkeyn (typed in chat field): Peninah, Hi. I wanted to throw your question back to you as I would be interested to know if IRC took the CHC training forward in any of your countries. We tend to lose track of what happens after a CHC trainings done as we don't get update after a consultancy.
-HLA MYAN: My question is when we do CLTS and CHC which is starting is the best way,start CHC or start CLTS first!
... and a related question:
-Omotomilola Ikotun: Is CHC done along side CLTS? I think it would be a perfect model if these are done hand in hand
Your answer in the webinar was (please expand if you like):
CHC is like a basket of topics; CLTS is one topic in the basket for intervention. It makes a lot of sense to have a correct entry with the community. CHCs take a lot of time to set up, enlisting members, talk to community leaders etc. When we start working through the topics and get to sanitation, that's when CLTS can come in. Sanitation is probably the most difficult thing you can ask the community members to do (like digging a pit). It is better to start with small incremental steps - slowly build up to the most difficult one (sanitation). So CHCs are started are first and then at thr right time, CLTS can come in.
-Henrietta: Is the focus of CHC primarily on ODF/ZOD? What standards are the latrines built to and would WHO? JMP accept these as imporved sanitation? I ask as in Uttar Pradesh there is the issue of building basic latrines with little focus on moving individuals and communities up the sanitation ladder.
Your answer in the webinar was (please expand if you like):
Once people understand the concept of why feces are dangerous, they will find ways to block access of flies. The sanitation ladder approach is very important. A lot of latrine drop holes in Rwanda are covered but there could be a crack in the floor next to the drop hole and the flies still get in... - this means peole haven't fully understood the concept. - Upgrading the latrines is very important. A lot of latrines are often very unsanitary... but rather than saying "build a VIP or nothing" we would say: start with small steps, e.g. dig a small hole and cover it after defecation - anyone can do that!
-darja.kragic: What is your experince/which approach would you take, when working with communities in (low income) urban areas?
Your answer in the webinar was (please expand if you like):
We have had a lot of interest from urban (peri-urban) areas. In fact a cholera outbreak in 2008 in Zimbabwe was our starting point - we used CHC in an emergency context there successfully.
Peri-urban areas: a lot of focus is on solid waste disposal, general environment, drinking water - we have had huge success with cleaning up the areas by the community members. CHCs provide a good interface with municipalities (councils), they bridge those gaps (which are caused by mutual lack of trust), and they help the councils to understand better how to deal with informal settlements in a constructive manner.
Questions from the chat field that were not addressed in the webinar:
- Christoph Leitner: Juliet, I very much appreciate this thinking in incremental steps and not in a desperate fixation on following pre-set concepts. Do you see this happening in other organisations, as well? Would you say there is a general move in that direction?
- toyaz3112.naik: Apart from educating people what else we can do?
- Thelma Arko: Juliet i am glad to know about community health clubs, will try to implement this approach in slums in Ghana, what suggestions will you give?
- HLA MYAN: How can we pick-up not success CLTS to achieved done continiuos with CHC is can possible? (I don't understand this question)
Elisabeth
Freelance consultant on environmental and climate projects
Please Log in to join the conversation.
You need to login to replyRe: Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
Here are our responses to your questions:
1. Do the behaviours taught in the CHC groups focus only on health, or do they incorporate other aspects, for example the environmental sustainability of practices e.g. preventing pollution, potential for EcoSan practices? If not, is there scope for this?
Reply: The first 20 sessions in Phase 1 tend to address basic hygiene and primary health care - things women can do for themselves in the home. The 2nd stage can go on to address a whole range of topics, whatever is the focus of the programme. This can include environmental issues, deforestation, prevention of pollution, and of course any type of sanitation which is covered in the first phase. It is an ideal means of introducing any type of appropriate technology which is new to the area and that needs to be promoted and managed. eg a new type of water filter. This is because the group can help each other to do village level operation and maintenance. eg emptying ecosan latrines at schools can be done by the parents in a CHC which is in the catchment of that school - particularly if there is also a school health club.
2. What are the most effective methods for monitoring the outcomes of community health club interventions? Interviews/surveys about habits and practices, observation of changed practices, etc?
Reply: Africa AHEAD has been refining a spot observation tool, which we call a 'household inventory'. This is a simple survey which we have got going on a cell phone. A field worker can visit the household and note all the hygiene enabling facilities and rate the household in terms of good, average or high risk. We use 10 main indicators and each of these has five sub indicators all of which are empirically observable. We do not trust reported responses. The presence and usage of facilities are used as proxy indicators of changed practices. We do a base line and a post intervention survey using the same tool and compare the uptake. This will soon be available for other organisations if they want us to provide quality assurance. We are doing this to enable scale up whilst trying to set certain standards of excellence. I am sure interviews and qualitative methods are also useful but more difficult to make comparative assessments.
3. From my fairly limited knowledge of the sanitation sector, CHCs seems to be less widespread than some other approaches to sanitation promotion (e.g. CLTS); are there reasons for this? Is the approach widely applicable?
Reply: Yes, you are correct. Whilst my husband Anthony Waterkeyn and I, have been writing and advocating the CHC Model since 2005, Africa AHEAD is a small organisation and we lack the capacity and the support to role this out by ourselves. We work with other NGOs and provide training in the CHC Model but it is a slow process and there is little institutional memory in INGOs so often our efforts are reversed when the next consultant comes along with their own ideas!
In some countries, such as Rwanda, Unicef and USAID have supported the model through Ministry of Health and it has gone to scale in a national programme with a CHC now established in almost all the villages in the country. However, in most countries Unicef has promoted CLTS so single-mindedly that it appears they have resisted even looking into alternative models. The reasons they have neglected to pick up on the efficacy of the CHC are unclear. There seems to be a sort of cynicism that our claims could not possibly be correct. In some countries there were individuals who wilfully refused to consider the approach as it appeared it was in conflict with the methodology of choice which was CLTS.
In other countries Unicef, which very often controls the WASH sector, had no exposure to it, and it was just ignorance of any alternative.
There is a lot of professional jealously that has held back the expansion of the CHC Approach, so it has been a bit of an uphill battle to influence the sector. However it seems that now the tide is turning and many stakeholders in the WASH sector are beginning to look for other models to affect behaviour change. People who are trying to solve the issue of sustainable sanitation are realising that CLTS was far too 'quick and dirty', and that much more effort is needed to follow up with communities to stop them back sliding. The approach has been successful wherever it has been tried by Africa AHEAD and there are ample case studies on our website.
www.africaahead.com/project-type/rural-chc-projects/
At the end of this year the RCT on the CHC in Rwanda, funded by Gates, will be out and perhaps will shed more light on how CHC compare with other models of behaviour change. Meanwhile we continue to reach out to whoever is listening!
Many Thanks for taking the trouble to get this clarification!
Juliet Waterkeyn
Chief Executive Officer.
AFRICA AHEAD
Applied Health Education and Development Empowering Communities for Sustainable Development
www.africaahead.com www.chcahead.com
Please Log in to join the conversation.
You need to login to reply- CaitlinMcC
-
Less
- Posts: 7
- Karma: 1
- Likes received: 1
Re: Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
1. Do the behaviours taught in the CHC groups focus only on health, or do they incorporate other aspects, for example the environmental sustainability of practices e.g. preventing pollution, potential for EcoSan practices? If not, is there scope for this?
2. What are the most effective methods for monitoring the outcomes of community health club interventions? Interviews/surveys about habits and practices, observation of changed practices, etc?
3. From my fairly limited knowledge of the sanitation sector, CHCs seems to be less widespread than some other approaches to sanitation promotion (e.g. CLTS); are there reasons for this? Is the approach widely applicable?
Thanks!
Please Log in to join the conversation.
You need to login to reply- SDickin
-

- User is blocked
- I'm a research fellow at the Stockholm Environment Institute and a geographer interested in environment health linkages, including how water and sanitation fit within the greater sustainable development agenda.
Less- Posts: 68
- Karma: 4
- Likes received: 26
Re: Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
-Henrietta: How were the 20 topics for community health clubs (CHC) decided upon?
-Bruce Southerland: In Rwanda are you working through or with local government health agent?
-Kumi: CHC sounds like an excellent approach. Regarding the latrines, what are club members expected to do with the collected waste over the long term (e.g. when the pit fills up).
-Penninah: It appears this is a great way to integrate various programs, how many organizations are you working with, have they documented successes? are they sharing and where can we find the documents?
-HLA MYAN: My question is when we do CLTS and CHC which is starting is the best way,start CHC or start CLTS first!
-Omotomilola Ikotun: Is CHC done along side CLTS? i think it would be a perfect model if these are done hand in hand
-Henrietta: Is the focus of CHC primarily on ODF/ZOD? What standards are the latrines built to and would WHO?JMP accept these as imporved sanitation? I ask as in Uttar Pradesh there is the issue of builidng basic latrines with little focus on moving individuals and communities up the sanitation ladder
-HLA MYAN: How can we pick-up not success CLTS to achieved done continiuos with CHC is can possible?
-darja.kragic: What is your experince/which approach would you take, when working with communities in (low income) urban areas?
-Christoph Leitner: Juliet, I very much appreciate this thinking in incremental steps and not in a desperate fixation on following pre-set concepts. Do you see this happening in other organisations, as well? Would you say there is a general move in that direction?
-Comment from Juliet Waterkeyn: Peninah, Hi. I wanted to throw your question back to you as I would be interested to know if IRC took the CHC training forwrd in any of your countries. We tend to loose track of what happens after a CHC trainingis done as we dont get update after a consultancy.
-toyaz3112.naik: Apart from educating people what else we can do?
-Thelma Arko: Juliet i am glad to know about community health clubs, will try to implement this approach in slums in Ghana, what suggestions will you give?
You can watch Juliet Waterkeyn's presentation and discussion in the webinar videos attached below:
and her powerpoint presentation is available here:
Please log in or register to see it.
Research Fellow
Stockholm Environment Institute
Stockholm, Sweden
This email address is being protected from spambots. You need JavaScript enabled to view it.
This message has an attachment file.
Please log in or register to see it.
Please Log in to join the conversation.
You need to login to reply- Elisabeth
-
- User is blocked
- Freelance consultant since 2012
Less- Posts: 3372
- Karma: 54
- Likes received: 932
Re: Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
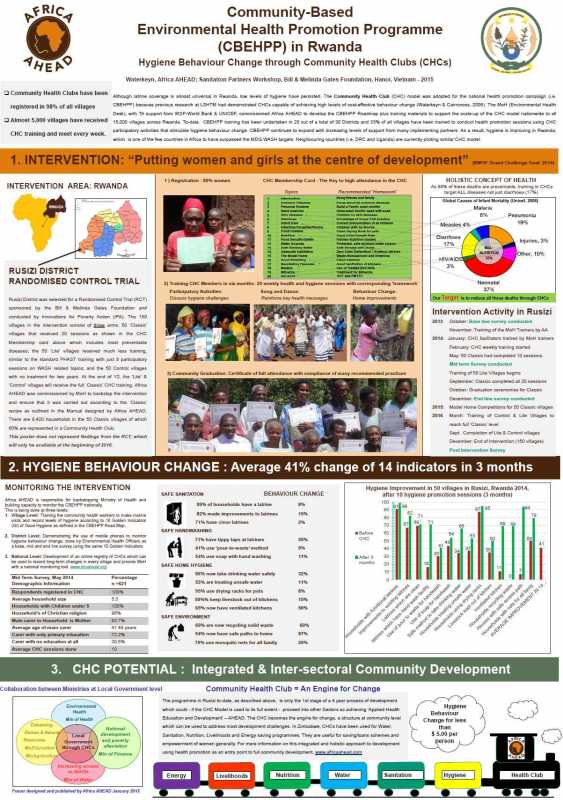
Anthony Waterkeyn attended the BMGF convening and presented this poster in Hanoi in January 2015 which sums up the approach and results from this project very nicely.
Visual impression:
The pdf file:
Please log in or register to see it.
The same pdf file in SuSanA library:
www.susana.org/en/resources/library/details/2183
Freelance consultant on environmental and climate projects
Attachments:
-
 PosterJuliet.jpg
(Filesize: 85KB)
PosterJuliet.jpg
(Filesize: 85KB)
Please Log in to join the conversation.
You need to login to replyMonitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)
Title of Grant: Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda
Name of lead organization: Ministry of Health with Africa AHEAD
Primary contact at lead organization: Dr. Fidel Ngabo / Joseph Katabarwa and myself at Africa AHEAD
Grantee location: Rwanda
Developing country where the research is being tested: Rwanda
Start and end date: June 30th 2012 – June 2016
Grant size: USD 925,020 (as per BMGF grant database )
Short description of the project:
The Ministry of Health (MoH) in Rwanda is currently implementing the Community-Based Environmental Health Promotion Programme (CBEHPP) which is in the process of establish Community Hygiene/Health Clubs (CHCs) in all 15,000 villages across Rwanda. The CHC model, as originally developed in Zimbabwe by Africa AHEAD (AA) in 1995, has in-built monitoring systems and tools . Although the CHC methodology has been adopted in a number of countries in rural and urban settings across East , West and Southern Africa over the past few years, Rwanda is the first country to be rapidly scaling up the model nation-wide. To date over 90% of the 15,000 villages in Rwanda have registered CHCs and over 5,000 have trained community members. By 2016, over nine million people (about 80% of the population) should benefit from CHCs if the programme is implemented as intended.
Since 2008, Arica AHEAD consultants have supported MoH to develop the CBEHPP Road Map (through WSP, 2008-2011) and the CHC Training Manuals (through UNICEF 2010-2011). It is now proposed that a practical monitoring system be established at village level in order to track hygiene behaviour change as the CHCs are established across the country. Africa AHEAD has been requested to assist in setting up monitoring procedures that will enable operational standards to be identified and demonstrated for the benefit of all CBEHPP implementing partners. A web-based ‘mobile research platform’ has been introduced to enable easy ‘real-time’ data collection and analysis using mobile phones, so building capacity for evidence-based policy-making within the MoH to ensure this national programme is rolled out at scale and implemented as cost effectively as possible. Rusizi district in Western Province of Rwanda was selected to demonstrate the ‘Classic’ CHC Model.
Within three years, 150 CHCs will have completed health and hygiene training that will benefit 15,000 direct CHC members (average of 100 members per Club) and with an estimated 75,000 direct beneficiaries (5 family members on average per household) with significantly improved hygiene facilities and behavioral practices in the home. Specific standards for the ‘Classic CHC’ will be established in order to provide a bench-mark for the national CBEHPP. In Year 1, a sample of 50 ‘Classic’ CHCs and 50 villages with a minimal ‘Light’ version of the CHC methodology was selected randomly, to be compared in Year 3 with 50 Control villages which will by then have received no treatment (i.e. neither exposure to the CHC nor training in health and hygiene). Monitoring the CHC model over three years will determine precisely how hygiene behavior can be improved to reduce the national disease burden in Rwanda and similar countries. Rusizi District will also be used for an in-depth evaluation study of health impact of the CHC approach. It will provide the first independent rigorous research of the CHC approach and will therefore be an important contribution to the international effort to identify the most cost-effective method to achieve sustainable and replicable hygiene behavior change at scale.
Goal:
To monitor the national Community-Based Environmental Health Promotion Programme (CBEHPP) and achieve cost-effective and sustainable hygiene behaviour change through implementation of the holistic and integrated CHC model to prevent common diseases.
Objectives:
There are five main objectives for this intervention:
1. To build capacity in MoH for cost-effective training of communities for hygiene behaviour change
2. To enable MoH to effectively monitor behaviour change through evidence-based data collection
3. To ensure functional and responsible communities exist in 150 villages in Rusizi district
4. To provide a demonstration on how hygiene behaviour change can be sustained
5. To demonstrate a cost-effective Change Model capable of improving family health at scale.
Research or implementation partners: Africa AHEAD / Innovations for Poverty Action
Links, further readings – results to date:
Our website: www.africaahead.com
Waterkeyn, J. & Cairncross, S. (2005). Creating demand for sanitation and hygiene through Community Health Clubs: a cost-effective intervention in two districts of Zimbabwe. 61. Social Science & Medicine. p.1958-1970.
www.africaahead.org/wp-content/uploads/2011/01/2005_SSM.pdf
Waterkeyn, J. and Waterkeyn, A. (2013)
Creating a culture of health: hygiene behaviour change in community health clubs through knowledge and positive peer pressure. Journal of Water, Sanitation and Hygiene for Development Vol 3 No 2. 144–155.
www.africaahead.org/wp-content/uploads/2...nowledge-in-CHCs.pdf
Recent presentation at World Water Week in 2014 (see also in this thread: forum.susana.org/forum/categories/5-clts...er-week-in-sept-2014):
Waterkeyn,J (2014) Going for ZOD (Zero Open Definition) in Zimbabwe, World Water Week, Stockholm 2014
Anthony A (2014) Seeing is Believing: CHCs in Rwanda. World Water Week, Stockholm, 2014
See in this link
Here you see myself presenting in Stockholm in Sept. 2014 (Dr. Juliet Waterkeyn, CEO, Africa AHEAD):
“I am Not Nothing Now” - How Community Health Clubs Empower Women
Here you see Anthony Waterkeyn, Chairman, Zimbabwe AHEAD, present at the same seminar.
"The 5x5 Strategy: Scaling up Community Health Clubs"
Current state of affairs:
Training of trainers was done in November 2013, and the training of CHC facilitators was done in January 2014. The CHC facilitators then returned to register members and village training sessions started with the community in February 2014. By May 2014 all 50 Classic CHCs were functional and there was an average of 77 members per CHC. Training sessions continued in the CHCs and by October 2014 all CHCs had completed the 20 sessions on target. Average attendance was higher than targeted 69% as against the target of 50%. Many households were making changes in their hygiene facilities and the mid term survey of 650 households shows significant improvement in all targeted activities.
Biggest successes so far:
The hygiene targets for this project were all set at 30% for end of Year 1. Five of the 9 indicators had exceeds targeted levels as shown below. Six months after the training had begun May 2014, the following levels were attained in 50 Classic CHCs:
• 70.6% have clean hygienic latrines
• 56.8% practice hand washing with soap after defecation
• 52.8% are treating unsafe water
• 85.2% have no open defecation
• 85.2% have no children’s faeces in the yard
• 75.1% use bath shelters for washing
• 41.3% have and use rubbish pits for solid waste disposal
• 32.2% yards are swept clean
• 94.5% have safe storage of utensils using pot racks or similar
Main challenges / frustration:
The project was designed for a randomized control trial and therefore implementation could not start until the base line had been done. The start up of the CHCs in Year 1 was meant to take place from June 2013. However the randomization of villages was not completed by the evaluation partner (IPA) until August 2013. This meant that MoH and Africa AHEAD could not begin any interaction with the villages until September 2013. This has delayed the implementation by 5 months. Thus the activities scheduled in ‘Year-One’ started for MoH and Africa AHEAD in October 2013 instead.
I am happy to answer any questions you may have about this approach and project.
Regards,
Juliet
++++++++
Further publications (see also our website www.africaahead.com):
- Maksimoski, N & Waterkeyn, A. (2000) The Community Health Club Approach in Informal Settlements: Case study from eThekwini municipality, Kwa Zulu Natal, South Africa . www.africaahead.com
- Okot. P, Kwame. V & Waterkeyn J. (2005) Rapid Sanitation Uptake in the Internally Displaced People Camps of Northern Uganda through Community Health Clubs. www.africaahead.com
- Ministry of Health- Environmental Health Desk (2010) Road Map for CBEHPP: Community Based Environmental Health Promotion Programme, Rwanda.
Chief Executive Officer
Africa AHEAD
UK Registered Charity: 1151795
www.africaahead.com
Please Log in to join the conversation.
You need to login to reply- Attitudes and behaviours
- Community-led approaches
- Monitoring Behaviour Change and Improved Health Outcomes through the Community Hygiene Club Methodology in Rwanda (Ministry of Health in Rwanda)







